Shoulder Replacement
What is the Shoulder?
- collarbone (clavicle)
- the shoulder blade (scapula)
- humerus, the largest bone of the arm.
- glenohumeral joint,
- acromioclavicular (AC) joint and
- sternoclavicular joint.
What is Shoulder Joint Replacement?
A shoulder joint replacement removes the painful contact between the worn humeral head and shoulder blade socket and replaces them with a new bearing surface that removes the arthritic pain. The surgery is performed under sterile conditions in the operating theatre under spinal or general anaesthesia +/- a nerve block. An incision is made over the affected shoulder to expose the shoulder joint.
The upper arm bone (humerus) is separated from the glenoid socket of the shoulder blade (Scapula). The humeral head which is arthritic is cut off.
The surgeon concentrates on the glenoid (socket).
- The arthritic part of the socket is removed and prepared to take the glenoid component.
- The glenoid component is then pressed into the socket.
- The upper arm bone is prepared to take the new humeral component.
The humeral component is then inserted into the upper arm bone. This may be press fit relying on the bone to grow into it or cemented depending on a number of factors such as bone quality and surgeon's preference.
- The humeral head component is then placed on the humeral stem. This component is made of metal.
- The artificial components are fixed in place. The Joint capsule is stitched together.
- The muscle and tendons are then repaired and the skin is closed.
Chronic Conditions Requiring Joint Replacement
- OsteoarthritisRheumatoid arthritis
- Post-traumatic Arthritis
- Rotator Cuff Tear Arthropathy
- Post-traumatic Arthritis
- Rheumatoid arthritis
- Avascular Necrosis (Osteonecrosis)
- Severe Fractures
- Failed Previous Shoulder Replacement Surgery
Before Shoulder Joint Replacement
- Consultation - During this consultation, Your doctor will:
- take a medical history : with emphasis on pain, disability and general health
- perform a physical examination : looking at range of motion and muscle strength.
- assess the joint’s range of motion
- Blood Test – can determine the condition of the bone and soft tissues of your shoulder
- Arthroscopy - link to Arthroscopy page
- Imaging Tests - In order to clearly understand the type of arthritis, integrity of the rotator cuff and bone loss, imaging scans are required.nature of any loss of the joint space or bone spur formation imaging scans are required:
- X-rays – These images help to determine the extent of damage in your shoulder. They can show loss of the normal joint space between bones, flattening or irregularity in the shape of the bone, bone spurs and the ball riding high on the socket after chronic tendon tears., and loose pieces of cartilage or bone that may be floating inside the joint.
- MRI - can create detailed images of both hard and soft tissues. An MRI can produce cross-sectional images of internal structures required if the diagnosis is unclear. It is the most accurate way of determining associated rotator cuff tears or muscle wasting.
- CT scans: are most accurate at detailing bone wear and can be used to create 3D models for surgical planning and implant placement.
- Ultrasound - can be a useful screen to check the integrity of the rotator cuff tendons allow the doctor to examine the inside of your affected area in motion.
Shoulder Joint Replacement Options
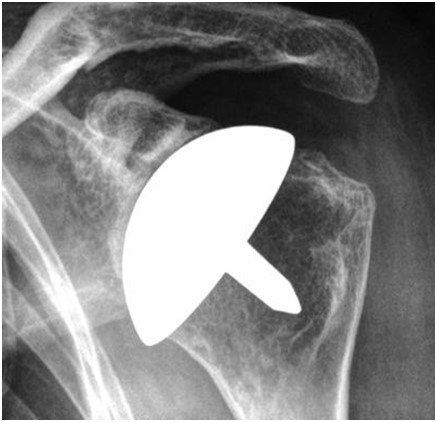
Total Shoulder Replacement
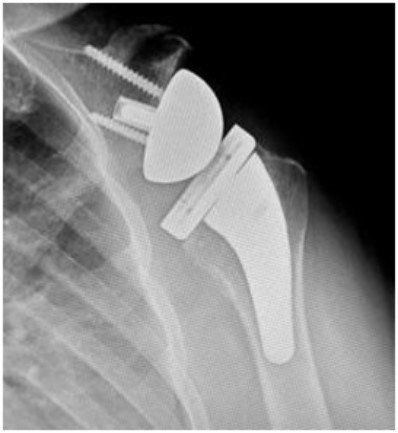
Stemmed Hemiarthroplasty
Resurfacing Hemiarthroplasty
Reverse Total Shoulder Replacement
- Allergic reactions to medications
- Blood loss requiring transfusion with its low risk of disease transmission
- Heart attacks, strokes, kidney failure, pneumonia, bladder infections.
- Complications from nerve blocks such as infection or nerve damage.
- Wound irritation - The patient’s scar can be sensitive or have a surrounding area of numbness. This normally decreases over time and does not lead to any problems with your new joint.
- Arm length inequality - On rare occasions it is simply not possible to match the arm lengths.
- Wear - All joints eventually wear out. The more active you are, the quicker this will occur.
- Failure to relieve pain - Very rare but may occur, especially if some pain is coming from other areas such as the spine.
- Unsightly or thickened scar - Scar tissue may be visible.
- Infection - Infections can occur superficially at the incision or in the joint space of the shoulder, a more serious infection. Infection rates vary; if it occurs it can be treated with antibiotics but may require further surgery.
- Shoulder Stiffness - Shoulder stiffness with loss of range of motion is a common complication that can be greatly minimized with strict adherence to your therapy program prescribed by your surgeon.
- Dislocations - Dislocations and/or subluxations with activity can occur. It is very important that you follow your surgeon’s guidelines for activity restrictions.
- Damage to nerves of Blood Vessels - Also rare but can lead to weakness or loss of sensation in part of the arm. Damage to blood vessels may require further surgery if bleeding is ongoing.
- Blood Clots (Deep Venous Thrombosis) - Blood Clots can form in the arm muscles and can travel to the lung (Pulmonary embolism). These can occasionally be serious and even life threatening. If the patient suffers arm pain, redness or swelling, or have shortness of breath at any stage, contact Your doctor
- Hemarthrosis - A condition caused by excess bleeding into the joint after the surgery is completed. This may require additional surgery to irrigate the joint. e surgery is completed. This may require additional surgery to irrigate the joint.
Surgery Preparation
- Your doctor will create a treatment plan and
- patients will also need to understand the process and their role. in it
- discuss any medications being taken with your doctor or physician to see which ones should be stopped before surgery
- do not eat or drink anything, including water, for 6 hours before surgery
- stop taking aspirin, warfarin, anti-inflammatory medications or drugs that increase the risk of bleeding one week before surgery to minimise bleeding
- review blood replacement options (including banking blood) with your doctor
- stop or cut down smoking to reduce your surgery risks and improve your recovery
Post Shoulder Surgery
- Pain medication will be provided to keep the patient comfortable.
- A bandage will be around the operated shoulder and the arm will be in a sling or brace.
- The sling will be worn for about 4-6 weeks to facilitate healing.
- The bandage will usually be removed 2448 hours post surgery and waterproof place dressings applied.provided by your surgeon over the area.
- It is normal for the shoulder to swell after the surgery. Placing Ice-Packs on the shoulder will help to reduce swelling. Ice packs should be applied to the area for 20 min 3-4 times a day until swelling has reduced.
- The patient will not be allowed to reach, lift anything over your head or anything greater than 1 kgilo or perform any resistance exercises for the first 6 weeks.
- Patients without support may require transfer to a respite facility to obtain greater independence befor returning home.
- 7-10 days after surgery Your doctor will see the patient monitor their progress and remove the sutures.